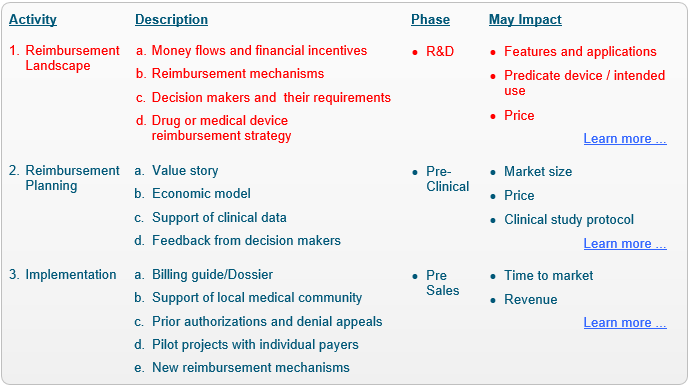
Reimbursement Consulting: Landscape.
Identifying reimbursement codes, coverage policies and payment rates, and developing the reimbursement strategy.
This is typically the first step in every reimbursement and health economics consulting project.
The purpose of this step is to understand the current reimbursement environment relevant for your device or drug.
(Back to main Reimbursement Process page).
Deliverables
Each of the deliverables below is conducted for each of the countries selected for the project.
a.
Follow the money:
Clarify money flows and incentives associated with the specific device or drug.
b.
Type of reimbursement mechanisms:
Identify the relevant type of coding systems, coverage policies, limitations and guidelines, relevant type of payment mechanisms and payment rates, applicable for the specific device or drug, or to any comparable products.
c.
Specific reimbursement mechanisms:
Locate any specific reimbursement mechanisms that could be utilized by the device or drug or recommend on whether new mechanisms will have to be developed and if so, which mechanisms (e.g., a new code, an expansion of a coverage policy, a new payment rate to an existing code or all of the above).
d.
Decision makers and strategy:
Identify the main decision makers, lay out the typical path towards obtaining third-party reimbursement, including milestones and typical timelines and provide an initial reimbursement strategy for the device or drug in each of the selected countries.
Methodology
In addition to purchasing access to secondary resources, we obtain primary reimbursement data, specific to your device / drug, by interviewing:
a.
Network exprts:
Our local specialists (in Europe and the US) in reimbursement and health economics.
b.
Potential clients:
Practicing physicians who may be using / administrating your device / drug.
Impact
The Reimbursement Landscape Report should be conducted as early as possible as it may impact the following:
a.
Product features:
The difference between being able to fit into existing reimbursement mechanisms and developing new ones is huge. If a new product can fit into an existing code, covered by payers and assigned with a satisfactory payment rate, reimbursement is practically immediate (following the regulatory approval). On the other hand, developing a new code, a coverage policy or just changing a payment rate, typically requires the company to provide substantial evidence through a costly and time consuming process. Therefore, design tweaks early in the product development stage that could let the product fit into existing mechanisms can make the difference between commercial success and failure.
b.
Product applications:
The same product may be covered for one application, thus fitting into existing reimbursement mechanisms, while not being covered for another. Selecting the right application for the product should also take into account the reimbursement consequences.
c.
Product intended use:
One of our clients applied for a regulatory clearance, indicating an intended use that substantially decreased the likelihood of reimbursement. Consequently, the company re-applied for the regulatory clearance, but this time, with a modified intended use. Needless to say, this delayed the launch of the product, resulting in substantial loss to the company.
d.
Selection of a predicate device:
A certain medical device company selected a very low priced device as a predicate device for its new and very sophisticated technology. The company went through the regulatory process quite quickly, however when we started discussing payment rates with payers, they were negatively impacted by the low cost predicate device. Despite tough negotiations, they were already biased and this new technology was priced below the expectations of the company.

